To: The Social Security Administration
From: Sean Smith, Tennessee
1.31.2020
A Disabled Citizen’s Comments on the Illegal Activities of Medicaid Programs and the Social Security Administration’s Irresponsible Stewardship. In relation to Docket: SSA-2018-0026-0092
I have doubts that the Social Security Administration’s proposed “Rules Regarding the Frequency and Notice of Continuing Disability Reviews” will serve “to maintain appropriate stewardship of the disability program”.
It’s hard for me to function day-to-day. I’m disabled and receive SSI and Medicaid as a consequence. I’m disabled by treatable medical conditions. Despite jumping through one administrative hoop after another I haven’t been able to access the care required to rehabilitate me. Why? Because the health plan administered through the Social Security Administration in my state is being permitted to engage in illegal activity. Many more medicaid & medicare plan members are subject to similar circumstances.
I and others experience this because medicaid health plans are excluding coverage of needed care and/or deny requests for care based upon policies and guidelines which are quite often not in compliance with state and federal healthcare mandates. Now, on top of that injustice is a proposal to increase the burden to recipients of SSA programs who are already overwhelmed by those illegal activities.
A burden that the SSA disability programs, Insurance Commissioners, Governors, and many others have abandoned the disabled to. It seems that dereliction of duty has become an acceptable behavior; to violate oaths, contracts, and fiduciary responsibilities has become so normal that even when it is explained to these individuals how their actions are illegal, they persist in illegal activity.
Police Officers claim it is a civil matter for attorneys. Attorneys say they don’t practice that area of law. Physicians claim it’s a problem between plan members and insurers. Insurers engage in misconduct to ignore or dismiss grievances and appeals. The Department of Commerce and Insurance points the finger to the Department of Labor. The Department of Labor points the finger back at the Dept of Commerce & Insurance. The Office of the Governor sends the issue over to the Department of Commerce & Insurance. The Directors of Tennessee’s Medicaid are a black void that offer no acknowledgement.
Ironically, all of this is occurring while the stated mission of the SSA, the purpose for which it receives federal funding, is to “assist the disabled” [1] in order to, “help rehabilitate the disabled so that they may return to useful employment” such that it “will advance the economic security of the American people.” [2].
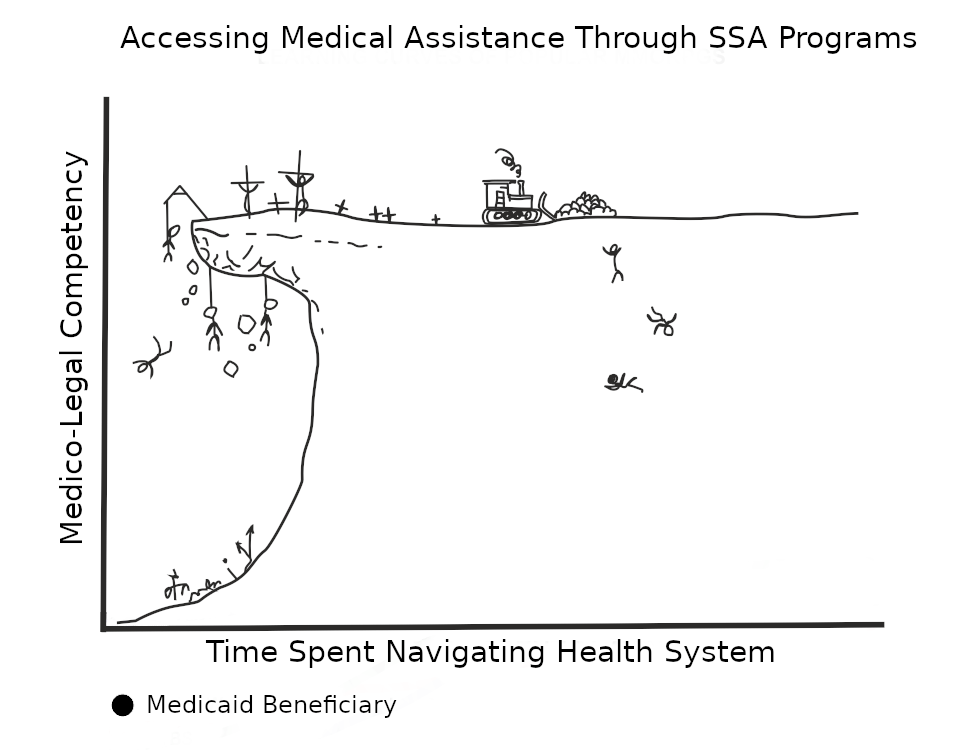
Yet, instead of providing the assistance beneficiaries require, SSA programs have been operating in a manner that increases the burdens upon beneficiaries in a misguided attempt to save money or to actively exploit them as commodities. So much so that it becomes a nearly full-time job trying to meet one’s needs through these programs, which is an absurdity given that these programs are meant to assist those too functionally impaired to maintain employment.
These actions do not save taxpayer dollars, but instead further increase the societal burdens we all pay the price for – people who could otherwise return to the workforce are abandoned to disabling medical conditions in a system that perpetuates continued disability. This undermines our economic security as a nation. Saying that there is gross mismanagement and waste occurring would be an understatement. I know some people would prefer to call it treason.
Prior to any discussion of the SSA implementing more extensive reviews of a persons disability status, there is a need to address the widespread misbehavior and illegal activities within SSA programs which are causing harm to beneficiaries of these programs and burdening our country.
Implementing more review is an ill-conceived idea because the existing review processes do not operate with integrity and have insufficient oversight to manage ongoing misconduct. It is, in fact, illegal for these organizations to place these existing burdens, let alone additional burdens which will worsen the existing ones, upon people who are disabled.
I would propose that if funds are to be further diverted to administrative costs they should be directed towards reviewing the activities of the departments tasked with reviewing claims for disability and requests for medically necessary care!
I take issue with the current proposal’s plan to classify people into the group “Medical Improvement Likely” as well as the proposed revisions of “the criteria we [SSA] use to assign a diary for a case”. I and others would likely improve if we received medical care appropriate to our medical conditions. Yet, the very rules and guidelines for the covered benefits provided by medicaid plans prevent that from occurring and the rules governing an SSI beneficiaries finances prevent disabled persons from using workarounds to acquire the funds needed to directly finance their medical care.
The widespread misbehavior and illegal activity within the medical insurance industry, both commercial and medicaid/medicare plans, set multiple barriers between patients and the care that they need to meet their medical needs.
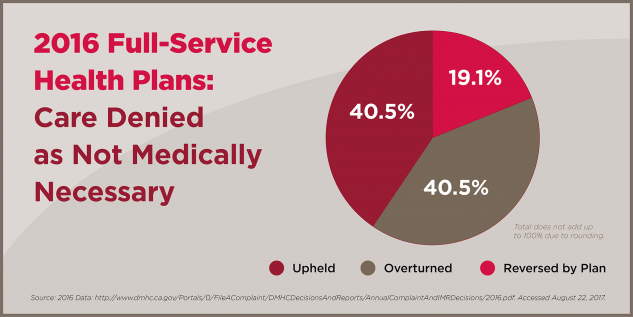
Grievances and Appeals are improperly investigated and marked as “case-closed”. Health Insurance “grievance systems are rife with abuse, says [California Nurses Association]”. The health plan grievance and appeals system is “deliberately an arduous, burdensome process…so that many are either unaware that they can appeal a care denial, or get so frustrated by the lengthy delay and bureaucracy that they stop fighting.” It has been observed that “64 percent of violations with monetary penalties were related to the insurer’s improper grievance process.” Plan members “get so frustrated by the lengthy delay and bureaucracy that they stop fighting.” It’s a “disgraceful game that insurance companies play with people’s lives.” [3] [4].
“Patient care denials are Exhibit A in how big insurance corporations amass huge profits by collecting premiums and then refusing to authorize needed care when recommended by a physician.”
“It is the purest example of how insurance companies prioritize their bottom line over patient need.” [3].
And yet, Medicaid plans are required to “assure that…care and services will be provided in a manner consistent with simplicity of administration and the best interests of the recipients” [42 U.S.C. §1396a (a) (19), 2020]. This obligates “State programs, like entities that administer these [medicaid] plans, to act with regard to the beneficiary interest in all phases of program operations.” and this obligation “can be thought of as extending to Federal program stewardship as well.”[5].
Yet, requests for care which are covered by medicaid health plans are wrongfully denied with disturbing frequency [6]. Misinformation is provided to members over the phone which delays or prevents access to care. Many of the diagnostic procedures and treatments required to accurately model and treat disabling medical conditions are excluded from coverage altogether or absent from provider networks despite the plan stating coverage is provided, particularly as it pertains to Sleep-Related Disordered Breathing, Temporomandibular Disorders, and other chronic pain conditions.
Many of the services which are covered by medicaid health plans are often reimbursed at a rate which does not allow the physician to deliver the therapy needed to treat the condition the health plan is claiming to provide coverage for.
The “mounting evidence suggests there are persistent gaps in the information [the Centers for Medicare & Medicaid Services] uses to estimate the costs of care for Medicare beneficiaries.” It is “a reimbursement system that fails to pay [doctors] for the true medical risks of their patients. ” [7].
Even when the rate of reimbursement is something physicians may find a way to work with, it is well known that one should expect that the claims one submits are quite likely to be wrongfully denied. In some instances it requires so much effort to repeatedly refile claims for reprocessing that it can make a physician’s practice unsustainable if they do not find a way to offset those costs.
I observe that as a consequence of these things physicians who adapt to this broken system become conditioned into a mindset wherein they are disposed to make statements like this, “…there is no point in fighting these people, we just have to do what they [medical insurers] tell us to do.” [a conversation between myself and a medical doctor].
The misconduct of health plans has become a pernicious blight upon our nation’s health system, consuming both patient and physician.
These medicaid programs receive federal funding for the purpose of fulfilling the SSAs mission of assistance and rehabilitation; “to furnish…rehabilitation and other services to help such families and individuals attain or retain capability for independence or self-care” [42 U.S.C. § 1396-1]. “The term “independence”, with respect to the diseases, disorders, and complications of aging, means the functional ability of individuals to perform activities of daily living or instrumental activities of daily living without assistance or supervision.” [42 USC § 242q-4(1)]
Yet there are entire patient populations who have their most basic needs left unattended to or poorly attended to: Pain, Breathing, Sleeping, Chewing, Digesting. Medicaid plans are not supplying the care necessary to allow beneficiaries to effectively treat many conditions which have a disabling influence upon ones Activities of Daily Living. This is not a small failure!
This is Fraud. Fraud committed against the Federal Government and the American People. Fraud that exploits our most vulnerable citizens.
It is fraud being committed by the administrators of medicaid programs and their third party administrators functioning as medical care organizations, for which it is the SSA’s duty to provide oversight. Thus, ultimately the misconduct of the SSA’s ancillary programs is the responsibility of the Social Security Administration, more so when matters are pointedly explained to the SSA in written format.
The SSA has a duty to “provide access to the services enrollees require to improve and maintain their health and functional status.”[42 U.S.C §1396. 2(D)]. They have a duty to do so “the degree to which Federal and State policies achieve their stated goals.” [42 U.S.C §1396 2(E)]. The SSA’s mandates are clear: The SSA is to facilitate rehabilitation, not interfere or impede it, and certainly not in a manner which discriminates against and violates the rights of medically disabled persons.
Given the current state of dysfunction within the medical insurance industry and within SSA medicaid programs, I would extend that the current rules being proposed, if enacted, would lead to an increase in illegal activity which penalizes beneficiaries and increases the societal burdens SSA programs are tasked to alleviate.
The effort to classify beneficiaries as “Medical Improvement Likely” based upon the evidence present in published literature will create a situation where beneficiaries are reviewed in the expectation that improvement of their disability was “likely” despite being unable to receive the medical care which would allow improvement of the conditions contributing to or causing their disability.
Some beneficiaries under these conditions will have their disability become more severe due to an inability to receive the care that is indicated to be efficacious within the scientific literature and/or through clinical findings. Such persons will find it difficult to gather and provide the information required by those performing the review of their disability status. They will be placed under burdens, burdens that their disability can impair their ability to shoulder.
This increased severity of their disability is likely to remain insufficiently documented because of the illegal activities of the medicaid programs that obfuscate access to care from competent specialists who can properly diagnose the medicaid beneficiary. In addition, medicaid programs often utilize medical assessors who deign to determine the status of a condition without having the highly specialized training required to understand that condition. A behavior that is otherwise known as malpractice has been used to discriminate against medicaid beneficiaries.
For recipients too overwhelmed or impaired to fulfill the demands of reviewers they will lose their disability benefits. After these individuals have had their rights violated and been relegated to complete financial and medical destitution, they will then become a greater burden to friends, family, and their community, that is, assuming the support systems they have access to will allow their survival. Some persons have been observed die as a result of the illegal activities of medicaid programs and the SSA.
I will reiterate, the SSA’s core mission is “to assist the disabled.”
Discrimination and abuse is occurring within SSA programs. More so within the medicaid programs in which misinformation and other barriers are inserted between members and access to medical care. It would be irresponsible stewardship to expect the SSA’s new proposed rule to somehow be exempt from the misconduct plaguing the medicaid programs and permeating into other arms of the SSA.
I have found that the disabled have been left at a disadvantage and are not having their rights respected. The disabled are being mistreated by those whose duty it is to review their claim of disability [7] or their requests for medical care with integrity.
I wonder, since despite my best efforts I have yet been unable to find someone to enforce the patient protection laws and laws protecting the disabled and other vulnerable citizens, perhaps the day is coming where the wronged parties will be required to exhort their fellows to form a citizens militia to perform citizens arrests and force law enforcement and attorney generals to fulfill their duties and prosecute offenders.
I’m amazed at how dysfunctional the SSA and other organizations have become and the complacency and rationalizations offered by the individuals within these organizations. I will have no sympathy for what happens to those people when the consequence of their failures begin to exact a personal and professional cost that leads them to ruin and despair. In fact, I think it will be well-deserved and long-overdue. How dare the Social Security Administration and Medicaid programs exploit and abuse the disabled and fail to act when made aware of these illegal activities.
With Regard,
Sean Smith
Contact: ThePatientsSingularity@gmail.com
Web: ThePatientsSingularity.wordpress.com
References:
- Social Security Administration. (2005/2006). A Primer: Social Security Act Programs to Assist the Disabled. Social Security Bulletin. 66(3); 53-58
- Social Security Administration. (2018). Annual Statistical Report on the Social Security Disability Insurance Program, 2017. SSA Publication No. 13-11826.
- California Nurses Association. (Feb 7, 2018). 60-80% of Insurance Denials Overturned or Reversed When Taken to Independent Medical Review – New Data. National Nurses United. [web article]. Retrieved: https://www.nationalnursesunited.org/press/60-80-insurance-denials-overturned-or-reversed-when-taken-independent-medical-review-new-data
- Department of Managed Health Care. (2016). 2016 Annual Report. [web document]. Retrieved: http://www.dmhc.ca.gov/portals/0/FileAComplaint/DMHCDecisionsAndReports/AnnualComplaintAndIMRDecisions/2016.pdf
- Sara Rosenbaum, Patricia MacTaggart, Phyllis C. Borzi. (2006). Medicaid and Health Information: Current and Emerging Legal issues. Health Care Financing Review. 28(2); 21-29. Retrieved: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4194976/
- California Chronic Care Coalition. (March 14, 2019). State Regulators Overturn more than 60
percent of Health Plan Denials. [Web article]. Retrieved:
http://mypatientrights.org/stay-informed/state-regulators-overturn-more-than-60-percent-of-health-plan-denials/ - Kenton J. Johnston, Julie P. W. Bynum, Karen E. Joynt Maddox. (2020). The Need to Incorporate Additional Patient Information Into Risk Adjustment for Medicare Beneficiaries. JAMA. doi:10.1001/jama.2019.22370
- Anita Wadhwani, Mike Reicher. (Jan 6, 2019). Doctors speed through disability claims, make millions: 6 takeaways from our investigation. The Tennessean. [web article]. Retrieved: https://www.tennessean.com/story/news/investigations/2019/01/06/tennessee-disability-claims-denials-appeals-investigation/2473381002/
Regulations.gov Comment Tracking Number for This Letter: 1k4-9eqp-i5jj
One thought on “The Illegal Activities of Medicaid Programs: A Letter Submitted to the Social Security Administration on January 30th 2020.”